Electrocardiography EKG/ECG is a medical technology used by doctors to monitor the function and electrical activity of the heart. Typical uses are to determine heart rate, heart function and heart rate variability (HRV). Furthermore, some parameters of the EKG/ECG signal may also indicate other disease or illness elsewhere in the body.



Table of Contents
How does ECG Work?
Electrocardiography works by taking advantage of the tiny electrical signals emitted by our heart. These tiny electrical “pulses” originate from specialised cells in the heart that are responsible for the beat of our heart, the contractions our heart muscle makes to pump blood around our body.
As these pulses spread outward they can be sensed at the skin surface with specialised electrical sensors, or electrodes. The sensors convey the small signals to a device known as an electrocardiograph that displays and records these signals for later review. The signals can be processed simultaneously to give medical professionals a real-time indication of heart rate and general heart health.
How is ECG Done?
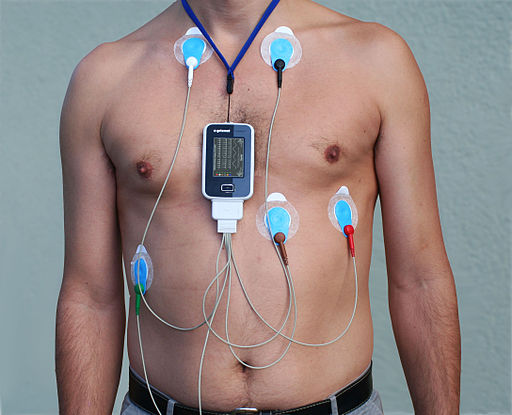
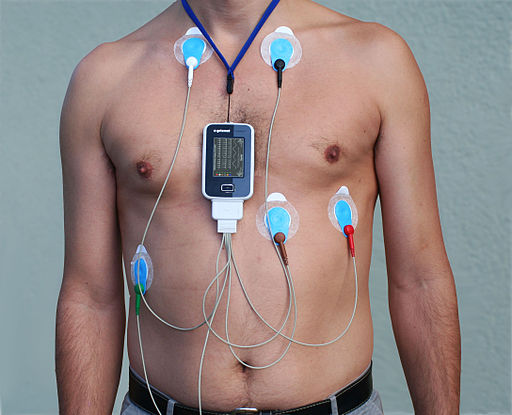
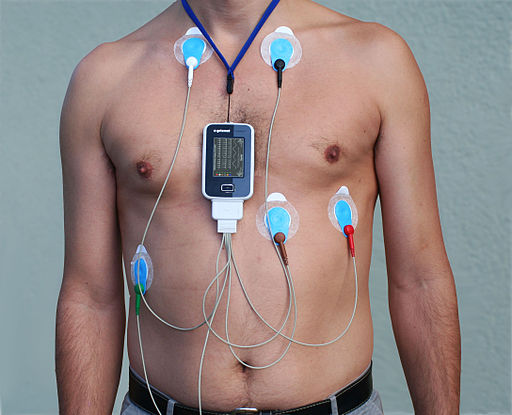
Electrocardiography is performed usually in a clinical setting. Sensors or electrodes, as they are known, are attached to you at various locations, typically on the chest area. A basic ECG requires just three electrodes.
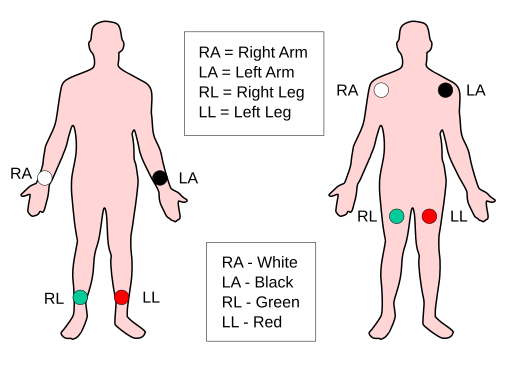
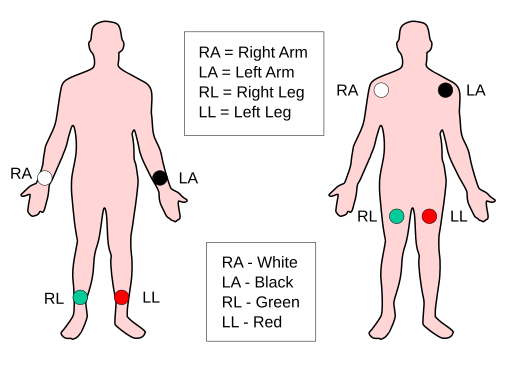
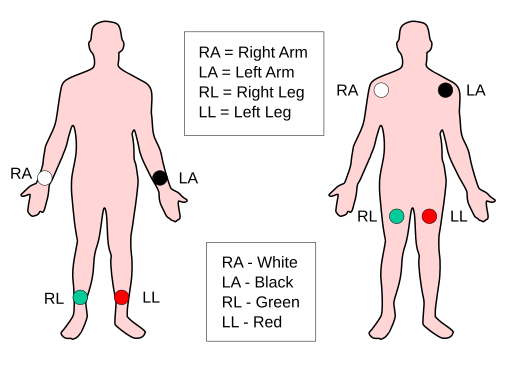
Two of the electrodes are placed either side of your chest just below the clavicle (collar bone) or on each shoulder on the right and left side. These are usually labelled RA (right arm) and LA (left arm) and can be coloured red and yellow or white and black respectively.
The third electrode acts as a reference to the other two and is placed either on the upper part of the left leg or on the lower most left rib directly below the LA electrode. The electrodes may also be placed on the wrists and ankles as demonstrated in the figure above.
Wires or “leads” are attached to these electrodes. It is the term “lead” that lends its name to the common name for the type of ECG monitoring that is performed, i.e. 3-lead, 4-lead, 5-lead etc.
Different numbers of ECG electrodes and leads are needed depending on the type of monitoring that is needed, more on that below.
The leads are then connected to the electrocardiograph that has specialised electronics designed to sense the very tiny electrical differences between each of the electrodes. These differences are amplified, processed and often displayed on an attached monitor. Clever computer software is able to determine your heart rate from the shape and repetitiveness of this signal.
When is ECG needed?
Firstly, the time you will definitely need an ECG is when you are in hospital, either in critical or intensive care. An ECG will also be applied when you are undergoing an operation and under general anaesthesia.
The NHS website (UK) has a good explanation of where ECG is used. Essentially, a doctor will order an ECG test whenever he/she suspects you might have a problem with your heart. Outward symptoms of a potential problem could be chest pain, dizziness, shortness of breath or sudden noticeable heartbeats (palpitations).
It is important to note that ECG’s are rarely used on their own as a definitive diagnosis tool. Instead they are employed alongside other tests to detect and diagnose heart conditions. The most common conditions detected with ECG are:
- Arrythymias – Where the hear rate is irregular, fast or slow
- Coronary Heart Disease – Where the blood supply to the heart in the coronary arteries becomes interrupted
- Heart Attacks – Where the supply of blood to the heart is suddenly blocked
- Cardiomyopathy – Where the heart muscle becomes enlarged and thickened.
ECG monitoring can be done in a clinic or hospital as the patient is resting on a bed. Commonly, patients will be fitted with a portable ECG device known as a Holter monitor. This device is designed to be worn by patients as they go about their normal daily routine. This is so that irregular and infrequent detectable abnormalities have a chance of showing up.
The Holter monitor can be worn for 1 to 2 days, this is a much longer period than typical clinical visits, making it much more likely that critical recordings are made.
Research in ECG also points to other diseases in the body that may be detected by the ECG by looking at specific changes in the different parts of the ECG signal. Prominent articles in this subject can be found to link diabetes mellitus, Lupus and others with ECG changes.
What is the Difference Between 3, 5 and 12 lead ECG?
The main physical difference between 3, 5 and 12(10) lead ECG is obviously the number of electrode/lead pairs and crucially the placement of electrodes.
Three lead ECG is common mostly on portable ECG units and is a good indication of immediate heart problems following an emergency situation, i.e. in the back of an ambulance, or on pregnant mothers in labour.
The process of electrical activity monitoring is more complicated than simply detecting the electrical pulses sent out by the heart. In matter of fact the heart signal, ECG, is better described as electrical vectors. An in-depth explanation of what these vectors are can be found here. Essentially there are three main vectors in 3-lead ECG, labelled nicely as I, II and III. These indicate 3 areas of the heart -the lateral(side) and 2 inferior(back) portions of the heart.
Using 3 electrodes allows us to take an average of these three vectors to arrive at what is known as the mean QRS waveform. This is what most people think of when they think of an ECG waveform. Different ECG waveforms will be seen at the different vectors however.
The 5-lead ECG is the preferred monitoring setup in critical or intensive care, and can monitor up to 7 electrical vectors (I, II, III, aVR, aVL, aVF and V). These 7 electrical vectors indicate different areas of the heart, and monitoring each area separately is useful when trying to determine if a patient is having a prolonged heart-attack, for example.
The 12-lead is used when diagnoses of heart attack or coronary problem are confirmed. The 12-lead ECG is in fact on a 10-lead setup, the name comes from the fact that 12 vectors of the heart can be simultaneously monitored (I, II, III, aVR, aVL, aVF, V1, V2, V3, V4, V5 and V6).
The increased level of detail in monitoring offered can help clinical specialists (Cardiologists) pinpoint the exact area of the heart that has the problem. In turn this will help them to make more determined diagnosis and design an appropriate treatment plan for the patient.
For a more comprehensive look at ECG we highly recommend the ECGpedia wiki.
When was ECG Invented?
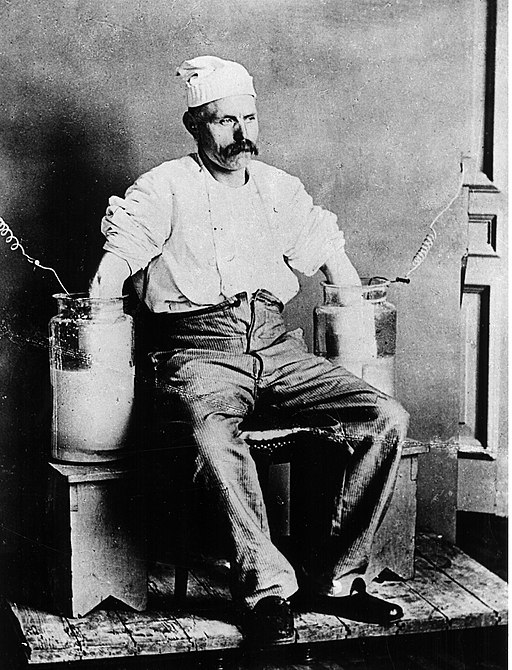
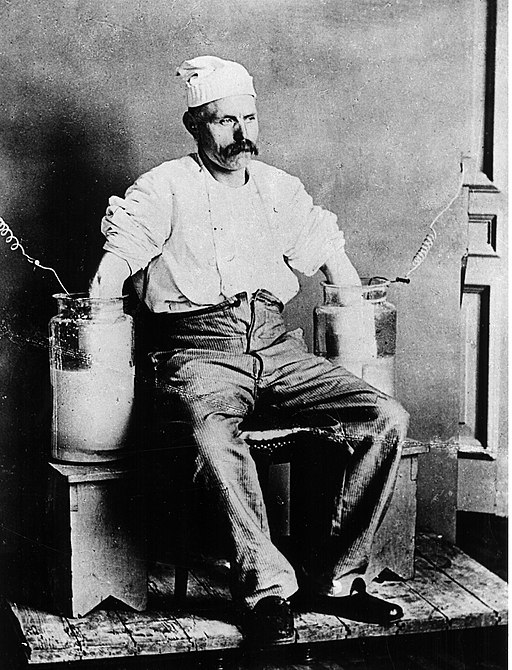
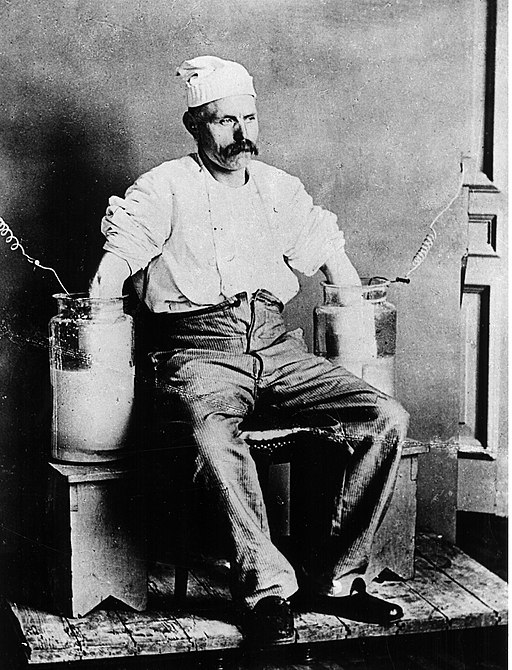
The first recording of an electrocardiogram was made by British Physiologist Augustus Waller in 1887 at St. Mary’s Hospital in London. Augustus also invented the first practical ECG machine that could record from the skin surface. Unfortunately the phenomena was regarded by Waller as a curiosity and he did not initially see the potential in diagnosing heart conditions.
Who Invented ECG?
It was Willem Einthoven, a Dutch Physiologist at the University of Leiden and Thomas Lewis, a British Cardiologist at University College Hospital London that showed the significance of Waller’s ECG discovery and how it could be used to diagnose heart disease.
Waller, Einthoven and Lewis therefore all contributed to the “invention” of ECG, with Waller being there first. Einthoven is mostly credited with his determination of the electrical axis of the heart and to improvements in the design of the instrumentation. For this work Einthoven received the Nobel Prize in Medicine in 1924. Lewis is considered to be the father of cardiac physiology, pioneering its use in the clinical setting.
ECG FAQ
Is ECG Accurate?
The ECG is considered to be the most accurate form of heart monitoring, and is accurate enough to detect a wide variety of heart conditions.
It is possible though to have a normal ECG trace and still have a cardiac condition. For this reason clinicians will rarely just rely on the results of an ECG for more complicated conditions, and why ECG is performed with other types of monitoring.
A common test performed alongside ECG is a n ultrasound of the heart, known as echocardiography.
How to Pronounce Electrocardiography
Electrocardiography is pronounced ELEC-TROW(as in crow)-CARD-IOG(as in fog)-RAFFY(think coffee). Below is a sound recording of how it is pronounced.
What is the difference between EKG and ECG?
Despite the different terms there is no difference between EKG and ECG. They are the same thing. The different abbreviation stems from the German (and other European) and English spellings of ElektroKardioGramm and ElectroCardioGram respectively. Some parts of the world adopted ECG, and others use EKG.
Is ECG and echocardiogram the same thing?
No it is not. An Echocardiogram is an ultrasound monitoring of the heart and uses different sensing technology. Echocardiograms are generally performed by specially-trained clinicians and sonographers, whereas ECG/EKG recordings can be recorded more simply with little training. Sometimes it may be confused because an ECG/EKG is often recorded simultaneously to aid in diagnosis.
How much does ECG cost?
This question requires 2 answers. Firstly, there is the cost of ECG equipment, then there is the cost to receive or have an ECG test. Both answers will vary by region and type, so all quoted figures are approximate.
Cost of an ECG device
For a dedicated ECG device prices can be anywhere in the ballpark of £50 to £5,000 ($60 – $6000). This is of course dependent mostly on the type of ECG machine, whether it is approved for clinical use and other functionality they have. Additional cost for the disposable electrodes also needs to be taken into account.
Cost of an ECG test
In the UK a private ECG test will set you back from between £55 – £150 depending on the clinic and the length of monitoring. The NHS will pay prices close to the middle of this, and residents of the UK in NHS care obviously will pay nothing directly. Typical non-insured prices of an ECG test in the US are above that of the UK Private sector (around $200).
Can I buy an ECG machine to use at home?
Yes, you can. Curious Cyborg does not endorse home testing of any kind unless under the instruction of a qualified physician. We will therefore not be linking to any devices here. If you are interested then please do your due diligence and at the very least speak to your doctor, do not rely on internet searches.
References
- https://www.nhs.uk/conditions/electrocardiogram/
- https://www.sciencedirect.com/science/article/pii/S2352646718301558?via%3Dihub
- http://www.biomed.cas.cz/physiolres/pdf/64/64_S559.pdf
- https://en.ecgpedia.org
- https://pubmed.ncbi.nlm.nih.gov/12766530/
- https://en.wikipedia.org/wiki/Augustus_Desir%C3%A9_Waller
- https://en.wikipedia.org/wiki/Willem_Einthoven
- https://en.wikipedia.org/wiki/Thomas_Lewis_(cardiologist)