The Photoplethysmogram was first observed in 1936, by Alrick B. Hertzman who coined the term “Photoelectric Plethysmograph” due to the fact that the technique relied on using a light source and photocell to observe the light interaction with tissue. Hertzman theorized the regular pulsations that were seen could only be caused by the changing volume of blood in tissue synchronous with the beating of the heart (Plethysmograph). The term has more or less stuck, now shortened simply to Photoplethysmography or PPG. This is the history of Photoplethysmography.
In 1936 an electronic instrumentation system was used to measure blood volume changes in a rabbit ear utilising a light source and light detector. At the same time recordings from human fingers was also made (Rolfe, 1979).
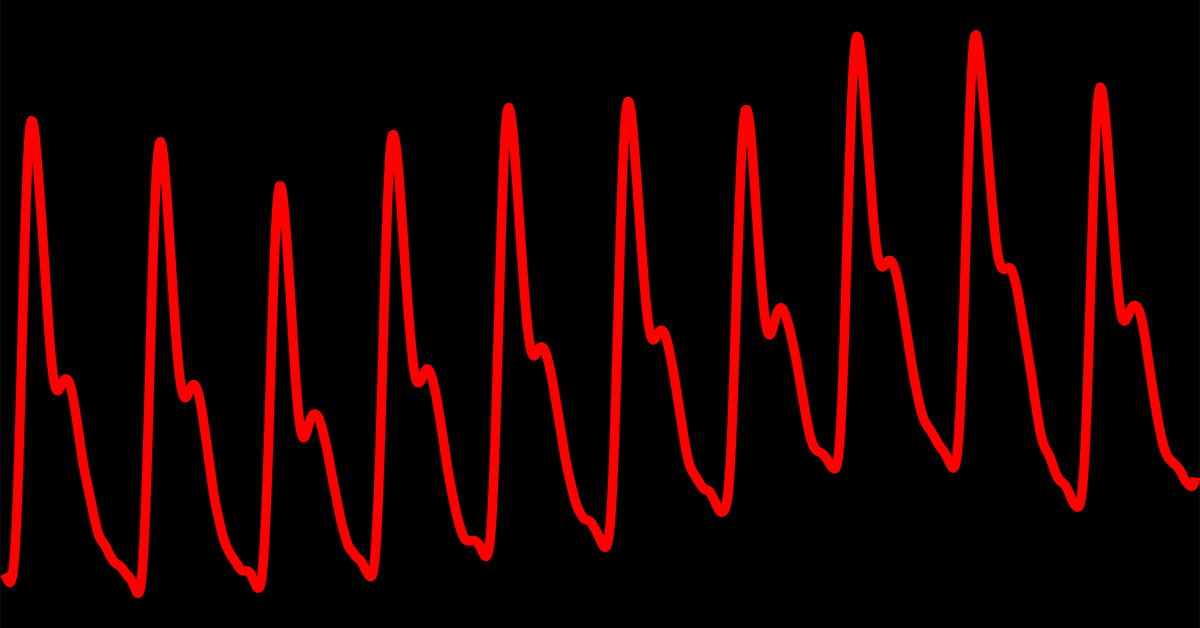
The Photoplethysmogram
Over 30 years of the earliest work in PPG was due to one individual and his affiliates, Alrick B. Hertzman. His first paper on photoplethysmography was published in 1937 (Hertzman, 1937); Hertzman coined the term “photoelectric plethysmograph” and made measurements using his apparatus to show blood volume changes induced by exercise, cold, and the Valsalva manoeuvre (forceful exhalation with the mouth and nose shut) (Rolfe, 1979).
The trace made by the PPG is known as the photoplethysmogram
The AC and DC PPG components described in our article on PPG were considered by Hertzman early on (Hertzman and Dillon, 1940), and he modified his apparatus to amplify these components separately. For the first time simultaneous measurements of both components were shown to provide more information on vasomotor changes (dilation or constriction properties of blood vessels) of the skin which was not possible previously.
The advancement of semiconductor technology reduced the size of early photo-detectors, whilst also making them more sensitive (Rolfe, 1979). New studies were conducted that were able to look at previous findings in more detail. Senay et al (1960) and Hertzman and Flath (1963) , were able to detect the onset of cutaneous vasodilation in fingers and forearms. In 1968 and 1969, Pollard, and Weinman et al respectively (Pollard, 1968, Weinman et al., 1969) both confirmed findings from Hertzman of the Valsalva manoeuvre causing changes in blood flow in the skin.
Our article on PPG described the general formation of the photoplethysmographic signal as observed with the arterial pulse, however as stated in that article there is debate amongst scientists as to the true origin of the signal which has produced experimental results that demonstrate the PPG as a far-more complicated signal.
Several key factors that affect the amount of light received by the photo-detector have been described (Moyle, 2002), these include;
- changes in the amount of blood under the probe
- red blood cell orientation
- red blood cell concentration
- rouleau formation
- local blood velocity
- separation of light source and light detector
- arterial inflow and venous outflow.
Notably it is the effect of the red blood cells that have produced some interesting studies. In 1967 D’Agrosa and Hertzman studied various small vessels, (frog mesentery, hamster cheek pouch and rat mesoappendix) using microscopic photoelectric photometry (D’Agrosa and Hertzman, 1967). The study looked at the varying opacity of the vessels during different inhibited situations, such as the injection of adrenalin, and they compared their results to that of others and concluded that the “opacity pulse” of arterial vessels is not volumetric in origin. A postulation was put forward that either the pulse is due to orientation and/or change in the concentration of red blood cells of the blood.
In 1981 Nijboer, Dorlas and Mahieu published results from a rigid tube experiment that make suggestions that for reflectance photoplethysmography the blood cell orientation did have an effect on detected light intensity (in vitro experimentation) (Nijboer et al., 1981). During systole it is suggested that the blood cells would align themselves perpendicular with the flow of the blood, and in diastole the alignment would be parallel. The cells would therefore act like miniature mirrors reflecting more light back towards the sensor during diastole.
However, the in vivo results showed that the reflection of light from the surrounding tissues dominates over the reflection of light from the red blood cells, thus, in vivo, the reflectance PPG is dominantly an absorption measurement, and it cannot be said for certain if this mechanism is a major contributory factor.
The knowledge and application of PPG is the primary driver of the technology in Pulse oximeters, an invaluable medical tool that became a part of standard clinical monitoring not long after its invention. To learn more about pulse oximeters you can read this article.
References
- ROLFE, P. 1979. Non-invasive physiological measurements, Academic Press
- HERTZMAN, A. B. 1937. Photoelectric Plethysmography of the Nasal Septum in Man. Proceedings of the Society for Experimental Biology and Medicine. Society for Experimental Biology and Medicine (New York, N.Y.), 37, 290-292.
- HERTZMAN, A. B. & DILLON, J. B. 1940. Distinction between arterial, venous and flow components in photoelectric plethysmography in man. American Journal of Physiology — Legacy Content, 130, 177 -185.
- SENAY, L. C., CHRISTENSEN, M. & HERTZMAN, A. B. 1960. Cutaneous vascular responses in finger and forearm during rising ambient temperatures. Journal of Applied Physiology, 15, 611 -618.
- HERTZMAN, A. B. & FLATH, F. 1963. The Continuous Simultaneous Registration of Sweating and Blood Flow in a Small Skin Area. Aerospace Medicine, 34, 710-713.
- POLLARD, J. A. 1968. A new photoelectric plethysmograph. Anesthesia and Analgesia, 47, 310-319.
- MOYLE, J. T. B. 2002. Pulse Oximetry, BMJ.
- D’AGROSA, L. S. & HERTZMAN, A. B. 1967. Opacity pulse of individual minute arteries. Journal of Applied Physiology, 23, 613-620.
- NIJBOER, J. A., DORLAS, J. C. & MAHIEU, H. F. 1981. Photoelectric plethysmography–some fundamental aspects of the reflection and transmission method. Clinical Physics and Physiological Measurement, 2, 205-215.