For an article of what pulse oximetry is, and how it works, see our other article “What is Pulse Oximetry ?“. For a short lesson of the history of pulse oximetry please continue reading!
Table of Contents
Haemoglobin Colour Change
The pigment that gives rise to the reddish hue in blood, haemoglobin, had been crystallized from various animals as early as the 1840s, but it wasn’t until 1862 that this substance was first reported to change colour when mixed with oxygen by the biochemist Felix Hoppe-Seyler (Hoppe-Seyler, 1864).
Hoppe-Seyler described the process of colour change as “beautiful” and noted two specific absorption bands, one at 560 nm and the other at 535 nm (both in the visible green band of the electromagnetic spectrum.)
In 1864 a physicist, George Gabriel Stokes, was the first to report the effect of treating blood with a reducing agent, observing that the two distinct bands merge to a broader absorption band with a peak roughly half-way between the peaks for the untreated blood (Stokes, 1864).
Crucially it was what Stokes did next in his experiment that demonstrated for the first time the dual-nature of the pigment, he reintroduced oxygen by shaking the blood with air, and the original bands reappeared.
This process could be repeated indefinitely, and Stokes concluded that the pigment could exist in two states of oxidation, distinguished by the visible difference in colour (red for the oxygenated state, and deep red/purple for the deoxygenated state). Stokes called these two substances Scarlet Cruorine and Purple Cruorine, but it is Hoppe-Seyler’s oxyhaemoglobin and haemoglobin, respectively, that we use today (Edsall, 1972).
The First Blood Oximeters
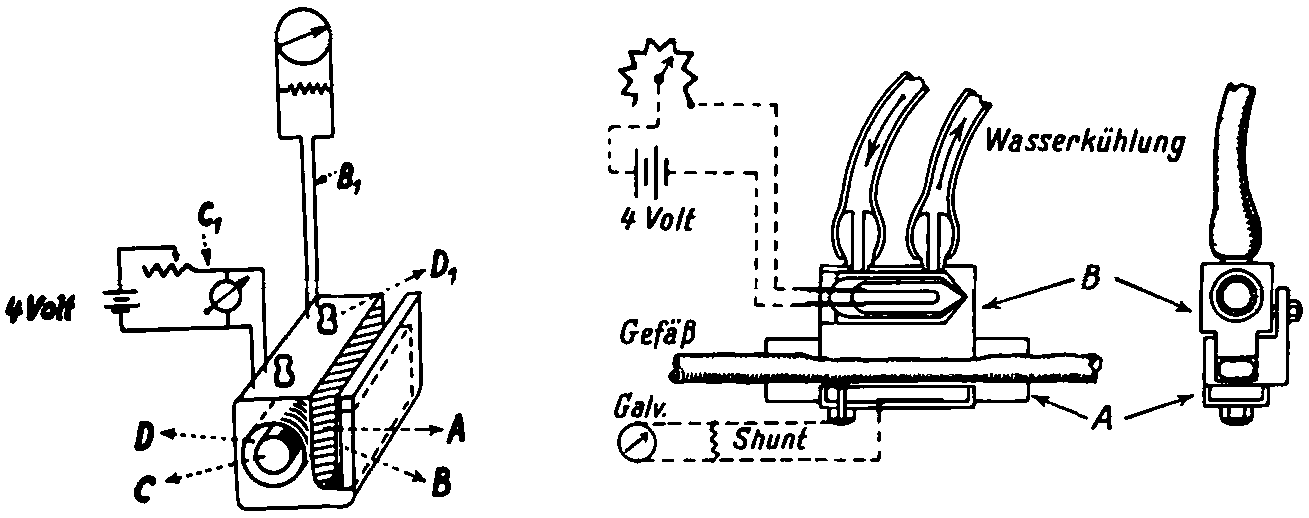
In the late 1920s Glenn Allan Millikan from the physiological laboratory in Cambridge built and tested, as part of his graduate thesis, a simple device for measuring the oxygenation of a haemoglobin solution. A diagram of the apparatus is shown in the figure below.



Light from a mercury-arc lamp passes through two filters (one purple and one yellow), so that when light goes from one end of the colour spectrum to the other there will be a significant change in the light being detected on one side of the differential photo-electric cell, the distribution of light reverses and thus so does the electric potential measured on the galvanometer.
The absorption spectra for oxyhaemoglobin and haemoglobin were obtained and calibration curves were derived. When samples of known saturation were then tested the overall accuracy of the device was approximately 4% for individual readings (Millikan, 1933, Severinghaus and Astrup, 1986).
In 1931 and 1934, Ludwig Nicolai and his associate Kurt Kramer performed the first oximeter experiments on living subjects (Nicolai, 1932, Kramer, 1934). Nicolai’s apparatus used the same Hg-ARC lamp as Millikan, and his protocol for measurement produced results that showed that the light transmitted through tissue, that had been occluded, would change linearly with time, when the logarithm was plotted.
This of course was as expected due to the oxygen consumption in a tissue. Kramer’s experiment used the principles of the Beer and Lambert Law by fixing the optical path length (2 mm cuvette) of an exposed, unopened blood vessel in a groove as shown below.
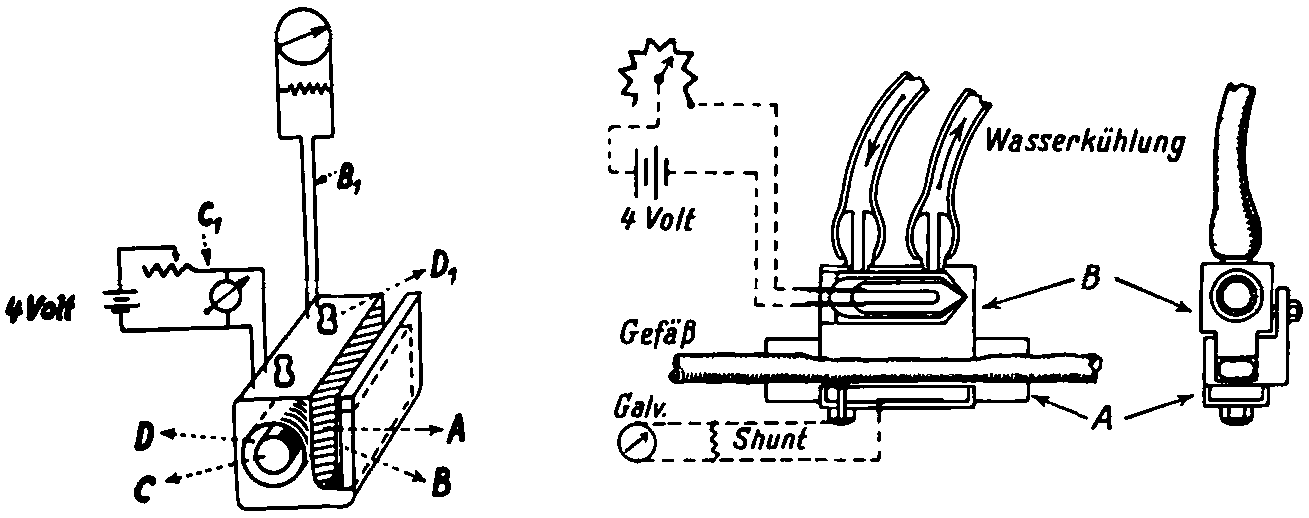
He changed his light source from the blue-green emission of the Hg-ARC lamp used by Nicolai and Millikan, and used an incandescent source with a red filter. Using a galvanometer, to make measurements, Kramer showed that saturation could be measured reproducibly and to an accuracy of ±1% (Severinghaus and Astrup, 1986).
The first oximeter system to use two spectral regions, one not affected by the other, similar to what is seen in today’s modern pulse oximeters, was developed by Karl Matthes and Franz Gross in 1939. The device was a red-infrared ear oxygen saturation meter, however it proved too large and inconvenient to use, and Matthes and Gross went back to reinvestigate the spectral properties of blood in order to improve the accuracy of their device (Severinghaus and Astrup, 1986).
The second-world war stimulated the need for an oximeter device that could be used in military aircraft in the unpressurized cabins of aircraft. In 1940 Millikan had developed a working device which, according to a report by his wife, could be used to control a servo system that would control the supply of oxygen to the mask of the pilot wearing the device.



In 1940, J. R. Squire from University College Hospital, London, added a new concept to the measurement procedure, by setting a zero point for the optical channels he used (one red, one infrared).
It was found that by compressing the tissue in the web of the hand, and squeezing out the blood, when the compression was released the change in absorption signal seen would only be due to the blood returning, thus the surrounding tissue could be eliminated in their estimation of oxygen saturation (Squire 1940).
Squire also introduced the idea of adjusting the red and infrared signal strengths, so that they would be equal with the inflow of blood, which should have made compensation perfect. This method was used by Earl Wood from the Mayo Clinic in his experiments, and anticipated the idea of the pulse oximeter (Severinghaus and Astrup, 1986).
In 1948 J. E. Geraci, under the guidance of Earl Wood at the Mayo Clinic, modified the Millikan ear oximeter to include an inflating balloon (Wood and Geraci, 1949). This was inflated to occlude the tissue in the ear and set a device “initial zero setting,” similar to Squire’s instrument. The balloon was deflated and the influx of blood to the tissue was used to determine the saturation reading.
By 1950 the Mayo group had reported use of the new oximeter in newborn infants, thoracic surgical operations, cardiac diagnostic procedures and exercise testing (Severinghaus and Astrup, 1986).
In the Hewlett Packard Journal of October 1976 (Merrick and Hayes, 1976), a review of the methods of oximetry, and a new multi-wavelength device were discussed. In this they highlighted the key limitations on the work done by Wood and those before him on ear oximetry. With regard to the ear oximetry technique they noted the following points;
- The bloodless ear is not truly bloodless
- The optical characteristics of the compressed ear differ from those of the ear in the normal state
- The optical path in the compressed state differs from that of the relaxed state
- Any movement of the earpiece changes the measuring circumstances, requiring a remeasurement of the bloodless state
- The forces required to secure the earpiece could interfere with the flow of blood.
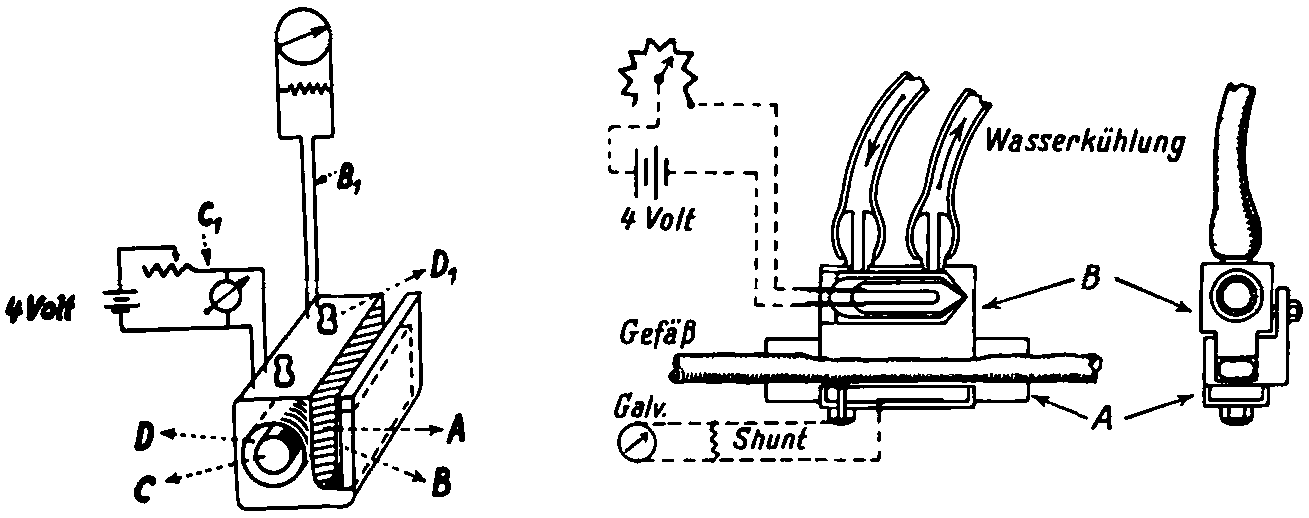
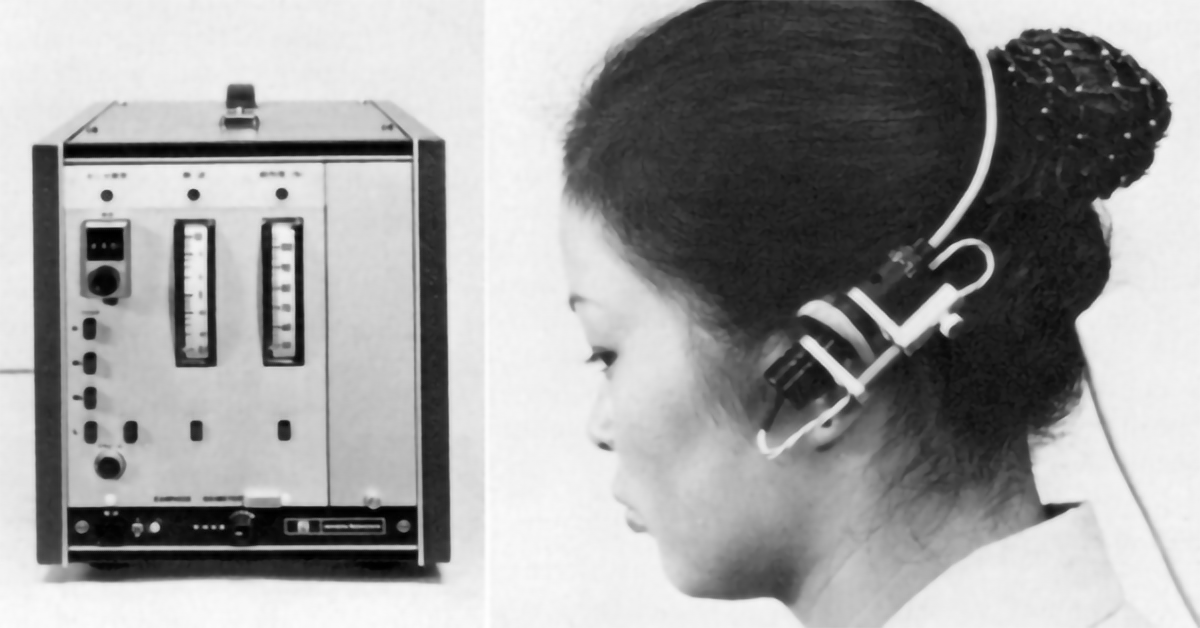
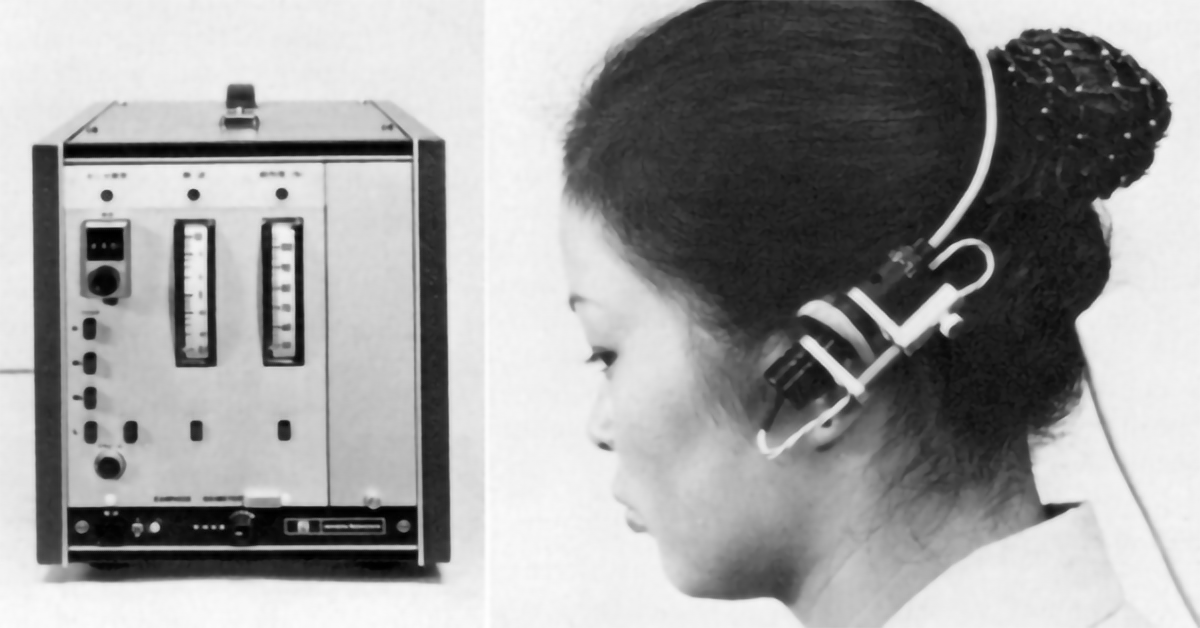
It was Robert Shaw, an M.D. from the Presbyterian Hospital in San Francisco that went to Hewlett Packard and showed that using a combination of measurements from several wavelengths it was possible to overcome these limitations. Feasibility studies were conducted, a product was designed and finally the achievement was the Hewlett Packard Model 47201A Oximeter (Merrick and Hayes, 1976).



In operation the device used a Tungsten-Iodine lamp with a rotating wheel of optical filters that cut the beam sequentially. This light was carried by a fibre-optic bundle to the emitting window of the earpiece. A returning bundle of fibres carried the transmitted light back to the instrument where a silicon photo-detector and amplifier was used to measure the returning light.
The rotating filter was used to synchronise reference and ear measurements so that the difference in each measurement for each wavelength could be compared, measured and digitised by an on-board analogue to digital converter. An on-board computer then made the calculation of oxygen saturation.
The Birth of the Pulse Oximeter
The pulse oximeter, as we know it today, was conceived in December 1972 by the Japanese Scientist and Engineer Takuo Aoyagi (Nihon Kohden Corporation, Japan).
Takuo Aoyagi was observing his cardiac output experiments and noticed the pulsation of the photoplethysmography (PPG) trace from his detector. He used this PPG to selectively determine just the arterial oxygen component, thus pulse oximetry was born.
In a self-review of his discovery (Aoyagi, 2003), Aoyagi makes it clear that the majority of his research was based on work done by the likes of Wood and Squire, even going as far as obtaining a Wood ear oximeter that they could study. The principles of operation of the pulse oximeter are detailed below, however it was in 1974 that the invention of the pulse oximeter was disclosed to the Japanese Society of Medical Electronics, and the OLV-5100 went to market.
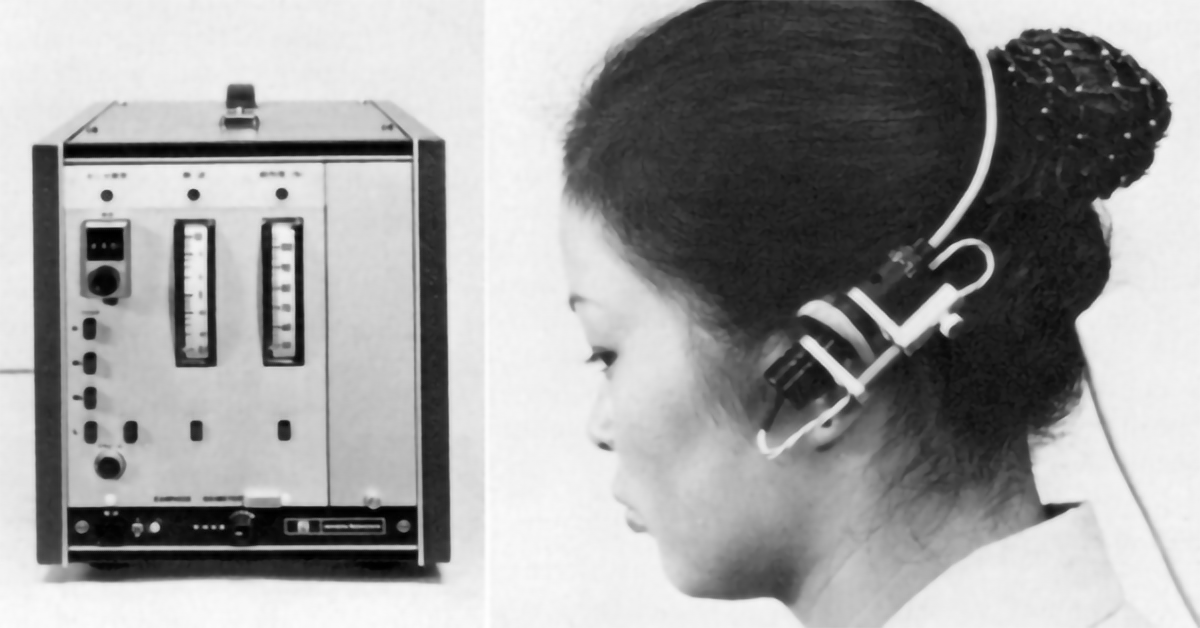
In 1979 the patent for the Pulse Oximeter was granted with Aoyagi named as inventor. Aoyagi left his research group for a period of eight years and it was in this time that the first commercially successful pulse oximeter hit the market, the Minolta OXIMET-1471 (1980), which used a conventional lamp + filters + optical fibres for the delivery of light to the tissue. In 1983 Nellcor Developed the N-100, which had replaced the light source and detector with LED’s and photodiode that could be mounted directly in the probe where the measurement was taking place. Aoyagi gives his thanks to Minolta and Nellcor for their development of the pulse oximeter, without them he says “the idea of pulse oximetry would have been buried” (Aoyagi, 2003).
References
- HOPPE-SEYLER, F. 1864. Uber die chemischen und optischen Eigenschafter des Blutfarbstoffs. Arch Pathol Anat Physiol 29, 233-251.
- STOKES, G. G. 1864. On the reduction and oxygenation of the colouring matter of the blood. philos Mag, 28, 391.
- EDSALL, J. T. 1972. Blood and hemoglobin: the evolution of knowledge of functional adaptation in a biochemical system, part I: The adaptation of chemical structure to function in hemoglobin. Journal of the History of Biology, 5, 205-257.
- MILLIKAN, G. A. 1933. A simple photoelectric colorimeter. The Journal of Physiology,79, 152-157.
- SEVERINGHAUS, J. W. & ASTRUP, P. B. 1986. History of blood gas analysis. VI. Oximetry. Journal of Clinical Monitoring, 2, 270-288.
- NICOLAI, L. 1932. Uber Sichtbarmachung, Verlauf und chemische Kinetik der Oxyhemoglobinreduktion im ebenden Gewebe, besonders in der menschlichen Arch Ges Physiol, 229, 372-389.
- KRAMER, K. 1934. Bestimmung des Sauerstoffgehaltes und der Himoglobin Konzentration in Himoglobinlslungen und himolysierten Blut auf lichtelektrischen Wege. Z Biol, 95, 126-134.
- SQUIRE, J.R., 1940. Instrument for measuring quantity of blood and its degree of oxygenation in web of the hand. Clinical Science,(4), pp.331-339.
- WOOD, E. & GERACI, J. E. 1949. Photoelectric determination of arterial oxygen saturation in man. J Lab Clin Med, 34, 387-401.
- MERRICK, E. B. & HAYES, T. J. 1976. Continuous, Non-Invasive Measurements of Arterial Blood Oxygen Levels. Hewlett-Packard Journal.
- AOYAGI, T. 2003. Pulse oximetry: its invention, theory, and future. Journal of Anesthesia, 17, 259-266.


Pingback: What are those Lights on the Bottom of My Watch? - Curious Cyborg
Pingback: What is Photoplethysmography – PPG, Why is it Important? - Curious Cyborg